Osteoporosis
What Is Osteoporosis?
The disease usually develops due to age and other factors and often progresses without any symptoms or pain. It is common to remain undiagnosed until you suffer a fracture. There are ways to prevent and treat osteoporosis symptoms.
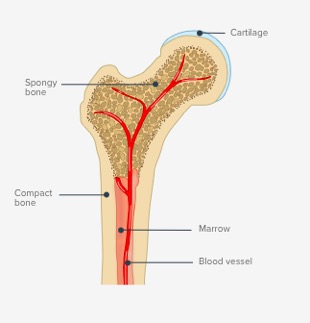
Anatomy
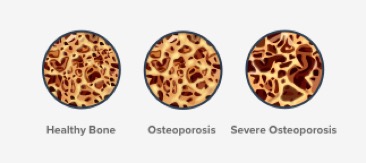
Your bones are made of living, growing tissue. The inside of healthy bone looks like a sponge. This area is called trabecular bone.
Bones are a major component of your skeletal system, which protects your organs. As you get older, your body replaces old bone tissue with new. When you are younger, you produce new tissue more easily. As you age, this process becomes slower and you even reach a maximum point.
Understanding Osteoporosis
Note: Did you know that osteoporosis translates to “porous bone”?
Who is at Risk?
Doctors do not know the exact medical causes of osteoporosis, but they have identified many of the major factors that can lead to the disease. While the majority of patients diagnosed with osteoporosis show many risk factors, it is possible to have no risk factors and still develop the disease. Some risk factors are out of your control, while others can be controlled.
Uncontrollable Risk Factors
- Your Sex: While osteoporosis affects both genders, it mainly affects women. Women over the age of 50 are four times more likely to develop osteoporosis. Women have less bone tissue and lose bone faster than men because of the changes that occur in their body during the first few years after menopause. These changes remain in the postmenopausal years. Currently, a woman’s odds of having an osteoporotic fracture are one in three.
- Age: The older you are, the greater your risk of osteoporosis. Your bones become thinner and weaker as you age.
- Body Size: Lower body weight and small or thin-boned women are at greater risk. Regardless of your body mass index, if you lose weight during the menopausal transition, you’re more likely to lose bone.
- Ethnicity: The genetics of osteoporosis are also reflected in the fact that different ethnicities and races have varying susceptibilities to the condition. Osteoporosis is more common in Caucasian and Asian women, especially older women who are past menopause. African American and Hispanic women have a lower but significant risk. Possible reasons could be bone structure differences such as greater peak bone mass, a slower rate of bone loss after menopause, and better quality of bone microarchitecture.
- Family History: Fracture risk may be due, in part, to heredity. People whose parents have a history of fractures also seem to have reduced bone mass and may be at risk for fractures.
Controllable Risk Factors
- Sex Hormones: Abnormal absence of menstrual periods (amenorrhea), low estrogen levels, and low testosterone levels in men can bring on osteoporosis. You may want to talk to your doctor about how to balance your hormones.
- Certain Medical Conditions: Celiac disease and Crohn’s disease can reduce the absorption of calcium and other nutrients needed for bone maintenance. If you have these conditions, it may be helpful to take calcium supplements.
- Your Diet: Eating more fruits and vegetables is always a good idea. Avoiding getting too much protein, sodium, or caffeine is advised by many providers.
- Calcium & Vitamin D Intake: A healthy diet preserves bone strength by providing key nutrients such as potassium, magnesium, phosphorus, calcium and vitamin D. Vitamin D is essential, since it helps calcium absorption from the intestines into the blood. If you don’t get enough calcium, your body will take it from your bones. A lifetime diet low in calcium and vitamin D makes you more prone to bone loss.
- Medication Use: Long-term use of certain medications, such as glucocorticoids and some anticonvulsants can lead to significant loss of bone density and fractures.
- Lifestyle: An inactive lifestyle or extended bed rest tends to weaken bones. Two types of exercise (weight-bearing and resistance) are known to be particularly important for countering osteoporosis.
- Cigarette Smoking: Smoking is bad for bones as well as the heart and lungs. Women who smoke lose bone faster, reach menopause earlier, and have higher postmenopausal fracture rates. The mechanism by which smoking causes bone loss isn’t known. Smoking may lower estrogen levels, or it may interfere with the absorption of calcium and other important nutrients.
- Alcohol Intake: Excessive consumption of alcohol increases the risk of bone loss and fractures. This may be a result of a toxic effect of alcohol on the bone forming cells. Some of the risk is also due to other poorly understood factors, which may include general deteriorating health and the increased likelihood of falling
Follow Us
Request An Appointment
Address: 3273 Claremont Way, Ste. 201, Napa, CA 94558
Phone: 707-603-1042
